
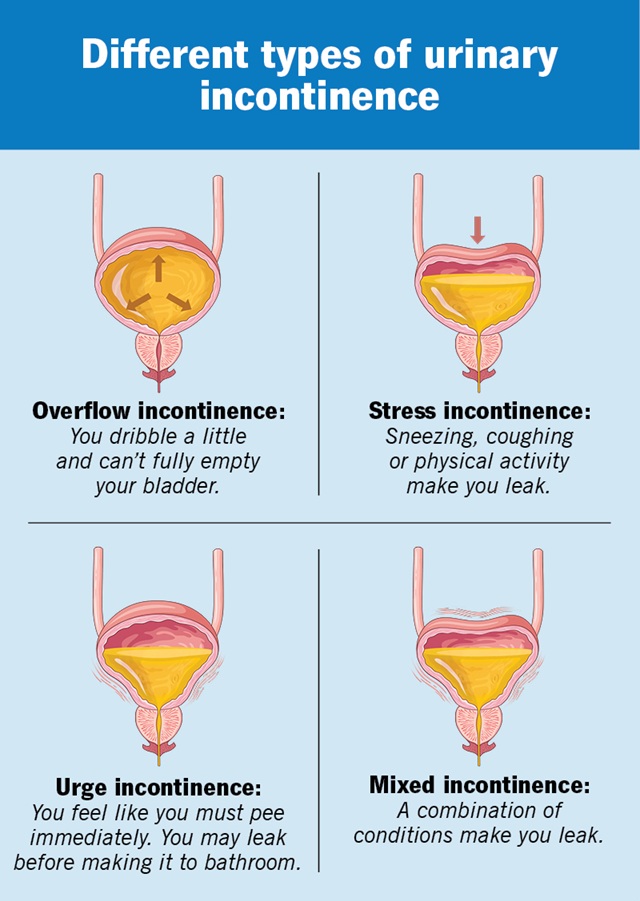
Approximately 30-65% of women experience urinary incontinence (involuntary loss of urine). Possible causes include injuries from childbirth, aging, certain vaginal surgeries, radiation therapy, and medications that interfere with muscle, nerve, and bladder function.
Just like any other system in your body, the urinary tract can stop functioning well. And that’s nothing to be ashamed of.
It’s not inevitable.
People used to think stress urinary incontinence came with the territory of aging. But the truth is, it’s a condition that affects both young women and old. Stress urinary incontinence is the most common type of urinary incontinence in women under 60 years old and can be related to a number of factors, including pregnancy, vaginal childbirth, strenuous exercise, menopause, and gynaecologic surgery. And unfortunately, ignoring it can’t help and won’t make it go away.
It’s treatable.
Stress urinary incontinence isn’t a disease; it’s a condition that can be successfully treated. And that’s the good news.
The choice between non-surgical and surgical treatment depends on the severity of the incontinence, the patient’s general health, how much the incontinence is affecting the quality of patient’s life, and most importantly, the patient’s ultimate goal.